Introduction
For colorectal cancer awareness month, we go behind the frequent calls for you to get screened. Let’s review the data and remind you why the disease itself is so devastating. This 2018 data is provided courtesy of the National Cancer Institute. They are based on statistics from SEER and the Centers for Disease Control and Prevention’s National Center for Health Statistics.
Cancer of the Colon and Rectum

First things first: The digestive system is made up of the esophagus, stomach, and the small and large intestines. The first six feet of the large intestine are called the large bowel or colon. The last six inches are the rectum and the anal canal.
Cancer that begins in the colon is called colon cancer. When it begins in the rectum, it is called rectal cancer. Cancer that starts in either of these organs may also be called colorectal cancer.
How Common Is Colorectal Cancer?
Compared to other cancers, colorectal cancer is fairly common. It is the fourth ranked with respect to new cases. It is the second ranked in terms of deaths produced.
| Rank | Common Types of Cancer | Estimated New Cases 2018 |
Estimated Deaths 2018 |
|---|---|---|---|
| 1. | Breast Cancer (Female) | 266,120 | 40,920 |
| 2. | Lung and Bronchus Cancer | 234,030 | 154,050 |
| 3. | Prostate Cancer | 164,690 | 29,430 |
| 4. | Colorectal Cancer | 140,250 | 50,630 |
| 5. | Melanoma of the Skin | 91,270 | 9,320 |
| 6. | Bladder Cancer | 81,190 | 17,240 |
| 7. | Non-Hodgkin Lymphoma | 74,680 | 19,910 |
| 8. | Kidney and Renal Pelvis Cancer | 65,340 | 14,970 |
| 9. | Uterine Cancer | 63,230 | 11,350 |
| 10. | Leukemia | 60,300 | 24,370 |
Colorectal cancer represents 8.1% of all new cancer cases in the U.S.
8.1%
For 2018, it was estimated that there would be 140,250 new cases of colorectal cancer and an estimated 50,630 people dying of this disease.
Prevalence of Colorectal Cancer
In 2015, there were an estimated 1,332,085 people living with colorectal cancer in the United States.
Number of New Cases and Deaths per 100,000
The number of new cases of colorectal cancer was 39.4 per 100,000 men and women per year. The number of deaths was 14.5 per 100,000 men and women per year. These rates are age-adjusted and based on 2011-2015 cases and deaths.
Lifetime Risk of Developing Cancer
Approximately 4.2 percent of men and women will be diagnosed with colorectal cancer at some point during their lifetime, based on 2013-2015 data.
Survival
How Many People Survive 5 Years Or More after Being Diagnosed with Colorectal Cancer?
Relative survival statistics compare the survival of patients diagnosed with cancer with the survival of people in the general population who are the same age, race, and sex and who have not been diagnosed with cancer. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
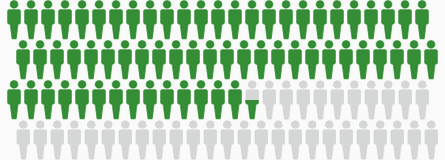
Percent Surviving 5 Years: 64.5%
Based on data from SEER 18 2008-2014. The gray figures represent those who have died from colorectal cancer. Green figures represent those who have survived 5 years or more.
Who Gets Colorectal Cancer?
Colorectal cancer is more common in men than women and among those of African American descent. The number of new cases of colorectal cancer was 39.4 per 100,000 men and women per year based on 2011-2015 cases.
Number of New Cases per 100,000 Persons by Race/Ethnicity & Sex: Colorectal Cancer
MALES
| All Races | 45.2 |
|---|---|
| White | 44.4 |
| Black | 55.5 |
| Asian/Pacific Islander | 39.3 |
| American Indian/Alaska Native | 45.1 |
| Hispanic | 39.7 |
| Non-Hispanic | 46.2 |
FEMALES
| All Races | 34.5 |
|---|---|
| White | 34.0 |
| Black | 41.9 |
| Asian/Pacific Islander | 28.0 |
| American Indian/Alaska Native | 39.2 |
| Hispanic | 28.6 |
| Non-Hispanic | 35.5 |
Percent of New Cases by Age Group: Colorectal Cancer
| Age Range | Percent of New Cases |
|---|---|
| <20 | 0.2% |
| 20-34 | 1.6% |
| 35-44 | 4.4% |
| 45-54 | 15.0% |
| 55-64 | 22.6% |
| 65-74 | 24.3% |
| 75-84 | 20.6% |
| >84 | 11.4% |
Colorectal cancer is most frequently diagnosed among people aged 65-74.
Median Age At Diagnosis: 67
Survival: Who Dies From This Cancer?
For colorectal cancer, death rates increase with age. Colorectal cancer is the second leading cause of cancer death in the United States. The number of deaths was 14.5 per 100,000 men and women per year based on 2011-2015 deaths.
Number of Deaths per 100,000 Persons by Race/Ethnicity & Sex: Colorectal Cancer
MALES
| All Races | 17.3 |
|---|---|
| White | 16.8 |
| Black | 24.4 |
| Asian/Pacific Islander | 12.1 |
| American Indian/Alaska Native | 20.2 |
| Hispanic | 14.7 |
| Non-Hispanic | 17.6 |
FEMALES
| All Races | 12.2 |
|---|---|
| White | 11.9 |
| Black | 16.1 |
| Asian/Pacific Islander | 8.6 |
| American Indian/Alaska Native | 13.6 |
| Hispanic | 9.0 |
| Non-Hispanic | 12.5 |
Percent of Deaths by Age Group: Colorectal Cancer
| Age Range | Percent of Deaths |
|---|---|
| <20 | 0.0% |
| 20-34 | 0.7% |
| 35-44 | 2.6% |
| 45-54 | 9.4% |
| 55-64 | 18.6% |
| 65-74 | 22.8% |
| 75-84 | 24.8% |
| >84 | 21.0% |
The percent of colorectal cancer deaths is highest among people aged 75-84.
Median Age At Death is 73
U.S. 2011-2015, All Races, Both Sexes
There’s More!
Read this Straight, No Chaser post on colorectal cancer screening. Please have this conversation with your physician. It could save your life.

Follow us!
Ask your SMA expert consultant any questions you may have on this topic. Also, take the #72HoursChallenge, and join the community. Additionally, as a thank you, we’re offering you a complimentary 30-day membership at www.72hourslife.com. Just use the code #NoChaser, and yes, it’s ok if you share!
Order your copy of Dr. Sterling’s books There are 72 Hours in a Day: Using Efficiency to Better Enjoy Every Part of Your Life and The 72 Hours in a Day Workbook: The Journey to The 72 Hours Life in 72 Days at Amazon or at www.jeffreysterlingbooks.com. Another free benefit to our readers is introductory pricing with multiple orders and bundles!
Thanks for liking and following Straight, No Chaser! This public service provides a sample of http://www.SterlingMedicalAdvice.com (SMA) and 844-SMA-TALK. Likewise, please share our page with your friends on WordPress! Also like us on Facebook @ SterlingMedicalAdvice.com! Follow us on Twitter at @asksterlingmd.
Copyright ©2013- 2019 · Sterling Initiatives, LLC · Powered by WordPress